Legacy prescribing is a common term in the world of deprescribing. It occurs when drugs should be prescribed for an intermediate-term (longer than 3 months, not indefinitely) but fail to get discontinued appropriately. In this post, we’ll dig deeper into the harmful effects of legacy prescribing, how it can lead to polypharmacy, prescribing cascades and unnecessary drug therapy.
Leg·a·cy
The long-lasting impact of particular events, actions, etc. that took place in the past.
Legacy is a tricky thing. It’s what we pass down from generation to generation. Some legacies are renowned, others traumatic.
In medicine, legacy prescribing can be viewed from the same lens. Prescriptions are passed down from specialists to general practitioners. Some medicines are essential, like receiving a timely inheritance. Other times, it’s a burden.
As a community pharmacist, it’s a unique vantage point to see these cases play out. Patients are prescribed medication by their specialists, and once their symptoms resolve, the medicine stays put. Their general practitioner endlessly repeats the prescription. As a result, patients find themselves entangled in a web of medications that may no longer be necessary, or worse yet, causing them harm.

Prescribing Cascades and Polypharmacy
Prescribing cascades occur when a medicine causes a side effect that gets misdiagnosed as a new condition. A new prescription medicine is then added to treat the side effect of the previous medicine.
This cascades into a chain reaction of ongoing side effects, which inevitably may lead to the addition of new prescription medicines, which can lead to drug interactions and an endless feedback loop.
The net result is usually polypharmacy, defined as being on 5 or more medicines for chronic health conditions. Polypharmacy is common in geriatrics for obvious reasons; as you age your health declines naturally. The issue is when we see prescribing cascades in middle-aged and younger patient populations. The longer you're taking a medicine, the more difficult it can be to reduce and reverse, especially for certain groups of medicines (like antidepressants).
Divorcing Medicines
Breakups are difficult. Whenever I encounter cases of polypharmacy or legacy prescribing, I reach out to the primary practitioner to inquire about the medicine at hand. The typical response I get back:
“Please direct your inquiry to the specialist. I did not prescribe this medicine.” (Not my problem)
“Specialist prescribed this medicine. Patient is to continue until follow up with specialist.” (Good luck, wait times for specialists is roughly ~ 3 to 42 months)
I’ll then proceed to reach out to the specialist. They haven’t seen the patient in ages and have transferred care back to the family physician. You can guess their response:
“Please refer to the family physician.”
This makes stopping unnecessary medications challenging. General practitioners have consult notes and instructions from specialists and may not feel comfortable stopping a medication they did not prescribe. On the other hand, specialists don’t have the same access and follow-up with patients to reassess their condition. In the end, the patient suffers the consequences of unnecessary drug therapy, adverse effects and risks of drug interactions.
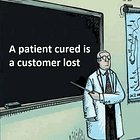
Convincing patients to change their medicines can present challenges as well. In our culture of medicine, we’re taught to always listen to our doctor (rightfully so). The doctor and pharmacist tell us we have to take our medicine, and we oblige. There is virtually no conversation or discussion on stopping medication, at any point in the patient-clinician interaction. The discussion is centred around symptom presentation, diagnosis then treatment options. This is where we need to improve.
Deprescribing and Simplifying Medication Regimens
To address the negative effects of legacy prescribing and polypharmacy, healthcare providers must emphasize deprescribing—the process of stopping medications that may no longer be beneficial or necessary. By reviewing each patient's medication regimen regularly, we can identify and eliminate legacy prescriptions, reducing the risk of drug-related complications and improving overall patient care.
Deprescribing needs to be established at the beginning of a patient’s clinical journey. Once a medication has been prescribed, it’s essential to establish clear goals of medication therapy with the patient. It’s important to be specific when outlining our goals of therapy. The clinician should work closely with the patient to identify specific parameters and symptoms to target, the expected and desired effects brought on by the medicine, and the timeframe and duration of therapy.
Our current models of care are static in nature. There needs to be a shift to a more dynamic clinical care model that emphasizes more follow-up and monitoring of progress. In my opinion, pharmacists need to step up to help facilitate this change. As stewards of medicine, we are in a unique position to initiate conversations with patients centred around deprescribing.
When patients get refills for medicine, it’s typical for pharmacists to sign off without question. Imagine if instead, we took that opportunity to inquire further into the patient’s history with the medicine, map out and assess their progress and help establish and realign the patient’s goals with their clinical care plan. There’s tremendous potential for pharmacists to add value and improve care, it’s up to us to evolve our practices away from dispensing and simply pushing pills.
Bottom Line
Reducing the burden of polypharmacy and legacy prescribing is crucial for promoting optimal patient outcomes. By streamlining medication regimens and deprescribing where appropriate, healthcare providers can enhance treatment efficacy, lower the risk of adverse events, and improve patient adherence. Open communication between patients and their healthcare team is vital to ensuring the most suitable and streamlined medication plan for each individual.
As our society becomes more and more medicated, it’s time we rethink our marriage to medicines. Deprescribing needs to be at the centre of that discussion.
Thanks for reading.
May you be happy and healthy.
SG
Build. Understand. Discipline. Stillness. “B.U.D.S” is written by me, Dr. Shawn Gill - I’m a pharmacist and Father of two boys. During the day, I work as a deprescribing pharmacist, helping patients get off drugs, safely and effectively. At night, I write this newsletter. B.U.D.S is a community that's focused on inspiring individuals to take account of their health and wellness, as well as reverse mental health and chronic disease. If you’d like to support this mission, please subscribe below. Much love. SG